Thoracic Spine Surgery
Thoracic spine surgery is a viable option for several spinal conditions that cause mid-back pain. The thoracic spine refers to the upper and middle-back portion of the spine. It joins the cervical spine and extends down about five inches past the bottom of the shoulder blades, where it connects with the lumbar spine. The thoracic spine is made up of twelve vertebrae, labeled T1-T12.
The design of the thoracic spine is meant to protect our heart, lungs, and other vital organs. It’s very stable and not meant to move much. The discs in the thoracic spine are smaller and better protected than in the low back and neck. Also, the spinal canal is narrowest in the thoracic spine, and therefore the spinal cord is at a risk for damage if a thoracic vertebra is injured.
Approximately 80-90% of people in the U.S. will experience back pain at some time in their life. Finding out how many people suffer from thoracic, or thorax pain can be difficult as there are different definitions of what thoracic pain is for different patients. According to a review quoted by Patient.Info, however, up to 20% of people with back problems may suffer from thoracic spine pain in their lifetime.
Causes
Up to 15% of individuals in the general population have asymptomatic thoracic disc herniations; 100 per 100,000 population will have symptoms. Each year there are 270,000 thoracic compression fractures caused by osteoporosis. The prevalence of scoliosis is 150 per 100,000 individuals in the U.S.
Conditions potentially requiring thoracic spine surgery include:
• Osteoporosis
• Scoliosis, a sideways curvature of the spine
• Compression fractures
• Kyphosis, a spinal disorder in which an excessive outward curve of the spine results in an abnormal rounding of the upper back
Symptoms that Indicate the Need for Surgery
Each year, an estimated 1.2 million Americans undergo spinal surgery. As each of the conditions that can require thoracic spine surgery is different, symptoms will vary. Back pain is the main symptoms of a thoracic herniated disc, which is one of the most common reasons for undergoing thoracic spine surgery.
Other symptoms that may indicate a person is in need of surgery include:
• Pain in the middle or the front of the chest
• Tingling and numbness
• Muscle weakness in one or both legs
• Increased reflexes in one or both legs
• Spasticity of the legs
• Pain that travels around the trunk of the body and into one or both legs
The symptoms of tingling, weakness, and numbness that affect an extremity occur from irritation and pressure on nerves. In addition, a thoracic herniated disc can lead to total paralysis of the legs due to spinal cord involvement.
If non-surgical treatments such as exercise, physical therapy, and medications do not relieve your pain, thoracic spine surgery may be necessary.
Thoracic Disc Herniations
The upper half of the thoracic spine is much less mobile than the lower section, making disc herniations in the upper thoracic spine rare. About 75% of thoracic disc herniations occur in the lower thoracic spine from T8 to T12, with the majority affecting T11 and T12.
Degeneration of the thoracic spine refers to changes in the discs between vertebrae that separate and cushion the bone. The discs lose their elasticity and thickness, and while the thoracic spine is the least likely segment of the spine to suffer such changes, discs do become displaced and herniate.
Thoracic discs can rupture suddenly due to too much pressure all at once on the spine, such as with a fall from a ladder or landing in a sitting position. Discs rupture from bending over, lifting something too heavy, force on the disc, or from repeated injuries that weaken the annulus fibers (the outer ring of the disc) over time. The material that ruptures into the spinal canal can put pressure on the nerves in the canal.
In addition, the chemical makeup of the nucleus is known to irritate the nerve roots. The pressure and irritation in combination can lead to pain, as well as weakness and numbness of an extremity. Most disc herniations in the thoracic spine squeeze straight back, rather than deflecting off to either side. As a result, the disc material is often pushed directly toward the spinal cord.
Diagnosis
Diagnosing the condition that may be causing your thoracic spine pain is completed through imaging studies, such as an MRI or CT scan. After a review of your MRI or CT scan, a complete physical evaluation and a consultation, your doctor can determine what is causing your pain.
After a diagnosis, a doctor will suggest the best surgical option for your condition.
Who is a Candidate for Surgery?
The goal of spinal surgery is to decompress the nerves that are causing the patient pain. After completing a full physical examination and reviewing your MRI, your doctor will determine if you are a candidate for spinal surgery. You may be a candidate for thoracic spine surgery if:
• Your pain is chronic or intolerable
• Nonsurgical treatments have not worked
• You have experienced loss of function
Every patient presents a unique challenge, which is why imaging is so important in determining if you are a viable candidate for thoracic spine surgery.
History of Thoracic Spine Surgery
The history of spinal surgery can be traced back to the 1950s when there were only a limited number of procedures and diagnostic tests. Almost all spinal surgery was completed through a large posterior incision. One of the first anterior cervical discectomies were performed during this era as well.
In the 1960s, the lumbar fusion was completed using metal hardware and new approaches to thoracic disc herniation were developed.
Open back surgery has typically been the standard for treating herniated discs, spinal stenosis, foraminal stenosis and other neck and back problems.
During a traditional open back surgery, a team of surgeons will make a large incision to access the problematic area of the spine. The surgeon may need to cut through tissue or move organs in order to reach the spine. The issues are addressed by hand and the surgeon will use stitches to close the incision.
Recovery for traditional open back surgery may last several months and could require the use of pain medication and a brace.
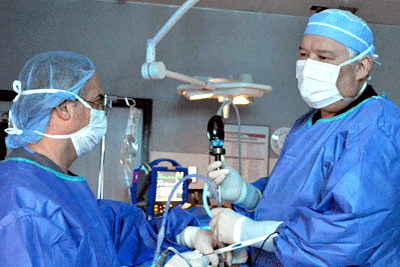
However, advancements have been made in thoracic spine surgery. The Bonati Spine Procedures, created and patented by Dr. Alfred Bonati, involve a small incision, no unnecessary muscle dissection, minimal recovery time and streamlined outpatient procedures, with much greater success rate.
Conservative Treatment and Alternatives to Thoracic Spine Surgery
In most cases, people with mild to moderate thoracic spine problems can manage their symptoms. Some non-invasive therapies and pain management options may include:
• Over-the-counter pain medicines, such as acetaminophen (for example, Tylenol) and nonsteroidal anti-inflammatory drugs (for example, Advil, Aleve, aspirin, and Motrin), to reduce pain. If these don’t get rid of your pain, you may need a prescription pain medicine that is stronger.
• Heat or ice to reduce pain and stiffness.
• Exercise to stretch and strengthen the muscles of your back, shoulders, and stomach.
• Physical therapy to help increase your flexibility, strength, and balance. Your physical therapist may teach you an exercise program so you can do it at home.
• Massage to help reduce muscle tension and pain and improve blood flow.
• Muscle relaxants to help reduce pain and muscle tension and improve mobility.
• Spinal manipulation to help relieve pain and improve function. It can range from massage and slow pressing to a quick thrust.
• Acupuncture
• Corticosteroid injections
Surgical Treatment of Thoracic Spine Problems
If conservative modalities have been ineffective, the Bonati Spine Institute offers an array of exclusive procedures for the treatment of thoracic spine conditions, including:
The Bonati Discectomy
If you have a bulging disc or a herniated disc, it may be pressing on your nerves. In a discectomy, the surgeon will remove the part of the disc pressing on the nerve.
The Bonati Facet Debridement of the Thoracic Spine and Facetectomy
There are joints in your spine called facet joints; they help stabilize your spine. However, misaligned facet joints can put pressure on a nerve. In many cases, growth called bone spurs can develop. A facetectomy involves removing part of the facet joint to reduce that pressure. Debridement means the surgical removal of torn, inflamed, contaminated, damaged or dead tissue. This technique may be used to treat painful facet joints.
The Bonati Foraminotomy/Foraminectomy
If part of the disc or a bone spur (osteophyte) is pressing on a nerve as it leaves the vertebra (through an exit called the foramen), a foraminotomy/foraminectomy may be done. A foraminotomy/foraminectomy is making the opening of the foramen larger, so the nerve can exit without being compressed.
The Bonati Laminectomy/Laminotomy
At the back of each vertebra, you have a bony plate that protects your spinal canal and spinal cord; it’s called the lamina. It may be pressing on your spinal cord, so the surgeon may make more room for the cord by removing part of the lamina.
Facet Thermal Ablation
A Facet Thermal Ablation is a laser eradication of sensory nerves causing pain. During a Bonati Facet Thermal Ablation (Rhizolysis), surgeons vaporize irritated and painful nerves around the facets of the vertebrae.
Recovery after Bonati Thoracic Spine Surgery
The Bonati Spine Procedures are advanced outpatient spine surgeries, which allow for faster recovery and greater success rate. Patients can go home the day of the surgery. Unlike open spine surgery or spinal fusions where patients had to remain in the hospital for days following their surgery.
The overall stress on the body is considerably decreased and blood loss is minimal. In addition, the risk of infection is much lower. Due to the nature of these procedures the movement of the spine is preserved, therefore, the formation of scar tissue is greatly reduced, and there are also less visible scars on the skin. Most importantly, with less damage to tissues of the spine, the potentially deleterious effects of spine surgery are minimized and the likelihood of injury to nerves both in the short-term as well as long-term is reduced. Another benefit of the Bonati Spine Procedures is that they may be performed on patients that were formerly considered poor candidates for spine surgery.
It is recommended that you begin a regimen of walking therapy as soon as possible after your thoracic spine surgery. Walking is a low-load activity, ideal for most people during their recovery from back surgery. It is the least harmful to your back, does not require any special equipment and provides the most benefits compared to other forms of exercise. Eventually, you’ll be able to return to your regular fitness regimen. By that time, you may appreciate the benefits of walking so much that you make it an integral part of your healthy lifestyle.
The Bonati Spine Procedures are performed outpatient, so no overnight hospitalization is required. The patient is administered a local anesthesia and conscious IV sedation so that he or she may remain awake during surgery and able to communicate with the surgeon. The incision is very small and dissection of muscles and disruption of tissue are avoided, along with scar tissue formation and extreme blood loss.
A Word about Spinal Fusions
Increasingly spinal fusions are being recommended to treat degenerative spine conditions. Although fusions are occasionally appropriate for cases of spinal instability, such as that produced by spinal fractures, the risks of spinal fusions to treat degenerative conditions such as disc herniations, spinal stenosis, and degenerative disc disease outweigh the rewards of the procedure.
• Thoracic spine fusion is an extensive surgery and the healing process takes a long time (about 3 to 6 months, and as long as up to 18 months).
• The spine fusion forever changes the biomechanics of the back and is thought to increase the stress placed on the other (non-fused) joints in the lower spine and possibly lead to degeneration of the adjacent levels of the spine.
• An instrumented fusion can fail if there is not enough support to hold the spine while it is fusing. Therefore, spinal hardware (e.g. pedicle screws) may be used as an internal splint to hold the spine while it fuses after spine surgery. However, like any other metal, it can fatigue and break causing scar tissue and compressed spinal nerves.
• A patient may experience recurrent pain many years after a spine fusion surgery. This can happen because the level above or below a segment that has been successfully fused can break down and become a pain generator.
