Spinal Stenosis
Overview
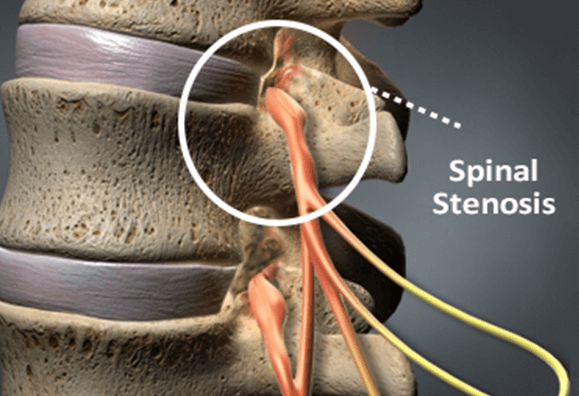
Spinal stenosis is a narrowing of the spinal column, which leads to the compression of the spinal cord or the spinal nerve roots. It often results in chronic back or neck pain, numbness, and weakness that radiates along the extremities. The Bonati Spine Procedures are designed to relieve the pressure on the nerves caused by this condition in order to alleviate the associated symptoms.
The primary goal of the procedures is to provide space for the constricted spinal cord and nerve roots. Decompression surgery for spinal stenosis is performed to alleviate pain related to the condition and to return any lost mobility or motor skills associated with the stenosis.
Our surgeons have performed thousands of successful procedures to treat spinal stenosis and its associated symptoms.
Anatomy
The vertebral column contains components critical to the stable functioning of the back and neck including the spinal cord, nerve roots, and vertebrae. Thirty-three vertebrae comprise the cervical, thoracic, and lumbar spine, as well as the coccyx and sacral, whose vertebrae are fused.
Each vertebra has three functional parts, the posterior, anterior, and spinal canal. The vertebral canal protects the spinal cord and contains fat, ligaments, and blood vessels. Vertebrae also have four facet joints, which connect each vertebra at the top and bottom.
On the back of each vertebra are bony projections that form the vertebral arch. The arch has two supported pedicles and two laminae. Under each pedicle, a pair of spinal nerves exits the spinal cord.
What is Spinal Stenosis?
Spinal stenosis is a medical term derived from the ancient Greek word “stenosis” meaning “narrowing”. Spinal stenosis is a disease of the spinal column that often leads to chronic back or neck pain.
In simple terms, spinal stenosis refers to the compression of the nerve roots or spinal cord compression due to the narrowing or impingement of the spinal canal.
If the narrowing of the spine affects the spinal nerve roots, the patient will experience radiculopathy, which is the radiation of pain down through the back and into the extremities.
Lumbar Spinal Stenosis
Lumbar spinal stenosis is caused by the compression of nerve roots in the lower back and often manifests as tingling, numbness or pain that radiates from the lower back and down to the buttocks or legs, also known as radicular pain or radiculitis. Neurogenic claudication is also a symptom of lumbar spinal stenosis and causes cramping or pain in the legs due to a nerve problem.
When the spinal canal or vertebral foramina narrow due to disease, degenerative arthritis, degenerative disc disease, or the degenerative aging process, lumbar spinal stenosis is usually diagnosed and subjected to applicable treatment methods. Spinal osteoarthritis destroys cartilage between vertebrae, promotes bone spur formation (osteophytes) and excessive growth of ligamentous structures. This is a result of the degenerative aging process. Also, while generally benign, synovial cysts may develop as a result of spine degeneration.
Lumbar spinal stenosis may also result from spondylolisthesis. This is when a vertebra slips forward onto the vertebra below. As the vertebral foramina narrows and spinal cord nerves suffer pressure from being compressed and restricted, lumbar spinal stenosis symptoms emerge and gradually worsen unless spine surgery is performed to remove pressure on nerves.
In addition to arthritis and spondylolisthesis, lumbar spinal stenosis may also be caused by tumors, infection or metabolic bone disorders associated with overgrowth of bone.
Delaying treatment for lumbar spinal stenosis may result in the symptoms getting worse, nerve damage, loss of function, myelopathy, urinary incontinence or loss of normal bowel functioning, etc.
Cervical Spinal Stenosis
Cervical or neck spinal stenosis occurs in the upper region of the spine, leading to a wide range of painful symptoms for those who suffer from this condition.
The condition is characterized by a narrowing of the spinal canal in the cervical region often caused by an impingement such as bone spurs, a herniated disc or bulging disc. Cervical spinal stenosis may occur with age and is sometimes a side effect of degenerative disc disease, osteoarthritis and rheumatoid arthritis.
Thoracic Spinal Stenosis
Thoracic spinal stenosis occurs in the middle portion of the spine caused by a narrowing of the spinal canal in the thoracic region of the back, often limiting a patient’s ability to move laterally or rotate. Stenosis of the thoracic spine is rare.
Who is Susceptible?
Though spinal stenosis can be a congenital condition or caused by injury or simply age, there are several other factors that could put you more at risk.
- Genetics
- Smoking
- Participating in high-impact sports
- A history of injuries
- Obesity
- Previous spine surgery
- Infections, diseases or tumors
Spinal stenosis is not only more common in those over the age of 50, gender could also be a risk factor as post-menopausal women are more susceptible due to osteoporosis.
Causes of Spinal Stenosis
Patients who suffer from spinal stenosis causes can be separated into those who inherit the condition and those who have acquired it over time.
Acquired Spinal Stenosis
Most patients seeking treatment for spinal stenosis suffer from the acquired version of the condition, as the narrowing of the spinal canal is a natural part of the aging process. Degeneration of the cartilage that provides a cushion for spinal joints exposes bone to friction and may result in bone spurs. As this bone on bone friction continues, the symptoms of spinal stenosis become more pronounced and the condition worsens.
In addition to the aging process, spinal stenosis is often induced by trauma to the back or neck that causes damage to the anatomy of the spine.
In general, the following may cause nerve compression or spinal cord compression and result in spinal stenosis:
- Herniated disc
- Bone spurs
- Bulging disc
- Spondylolisthesis
- Trauma and injuries
All spinal stenosis causes share the onset of osteoarthritis later in life.
Symptoms of Spinal Stenosis
Spinal stenosis symptoms may appear in the lumbar, thoracic and cervical parts of the spine. Depending on the location of the condition, patients may experience different symptoms.
Symptoms of Spinal Stenosis in the Lumbar Spine
- Sciatica
- Chronic lower back pain accompanied by increased pain and weakness in the legs when walking (possible sign of cauda equine syndrome)
- Pain is relieved by sitting , which returns when standing or walking
- General leg pain, tingling, weakness and numbness that radiates from the lower back into the buttocks and legs
- Lower back pain
- Lessening of discomfort when patient is leaning forward or sitting
- Worsening of pain when bending backward or standing
- Inability to walk moderate distances without experiencing pain
Symptoms of Spinal Stenosis in the Cervical Spine
Cervical spinal stenosis is far less common than lumbar spinal stenosis but can be more dangerous as the symptoms of the condition worsen. The compression of the spinal cord in the neck region often leads to painful symptoms across the entire body and can have a long-lasting negative impact on a patient’s quality of life.
The most common symptom reported by patients suffering from cervical stenosis is chronic neck pain. Neck pain is often accompanied by:
- Weakness
- Numbness or pain in the shoulders, arms or hands.
Symptoms of Spinal Stenosis in the Thoracic Spine
- Pain in the rib cage or internal organs
- Pain that radiates down the back of the legs
- Aching in the legs that leads to difficulty walking
- Problems with balance and coordination
- Problems with bowel or bladder function
Diagnosing Spinal Stenosis
Spinal stenosis may develop over time, which means many will not have any present symptoms until the condition is well developed. If it is caused by an injury, the symptoms may come on suddenly. If you are experiencing any symptoms of spinal stenosis, a physical exam and imaging studies can provide a correct diagnosis. During the physical exam, the doctor may test your muscle strength, reflexes, and balance. They will also ask questions about the location of your pain, what makes it better or worse, and about any treatment that has helped.
Exams & Tests
After a complete summary of your medical history and physical examination, imaging studies, such as an x-ray, CAT scan, or MRI will be done to see if the spinal cord or nerves are being pinched.
A myelogram, which uses dye to provide a high contrast image, will be done if necessary.
Treatment for Spinal Stenosis
Spinal stenosis treatment options range from conservative to the more aggressive and depends on the severity of the symptoms.
It is important to remember that although conservative treatment may be helpful in alleviating some of the symptoms of spinal stenosis, they do not address the underlying pathology driving the symptoms and are not curative.
surgery is required for long-term relief, when the symptoms are debilitating and non-surgical treatments fail to alleviate the symptoms.
Non-Surgical Treatment
First, doctors may pursue non-surgical treatments to help the patient find pain relief. This can include:
- Stretching
- Physical therapy to strengthen the neck and back
- Pain management, with over-the-counter or prescribed medications
- Massage therapy
- ESI’s
- Lifestyle changes
- Hot/cold therapy
However, in some patients, the pressure on the spinal cord creates symptoms far too painful and debilitating to lead a normal life. In these cases, a surgical procedure is necessary to correct the problem and relieve the pain.
Exercises for Spinal Stenosis
Physical therapists often direct patients to engage in back exercises developed to ease these symptoms. These back exercises usually include a combination of specific stretching and strengthening routines. Forward bending exercises increase the size of the compressed passageways providing temporary relief from pain and strengthening the surrounding muscles to improve stability.
Some other forms of exercise patients may engage in include:
- Stationary biking
- Walking
- Swimming
- Tai Chi
- Yoga
Before beginning any new exercise routine, speak with your doctor about what is safe for you to do.
Treatment & Self-Care
Along with conservative treatment, you may also complete some self care at home to reduce the pain. Some self-care methods may include:
- Topical pain medication (i.e. Icy Hot or Biofreeze)
- At-home massage therapy
- Non-steroidal anti-inflammatory drugs (NSAIDs)
- Correct your posture when sitting and standing
- Drink plenty of fluids
- Eat a nutritious diet
- Stop smoking and reduce alcohol use
- Maintain a healthy weight
Although each of these methods may help to reduce the symptoms, they do not get rid of the stenosis.
Surgery for Spinal Stenosis
The Bonati Spine Procedures relieve the pain caused by spinal stenosis and return the patient to normal activities within days. They are done at an ambulatory surgery center instead of a hospital. And performed under local anesthesia and conscious IV Sedation to avoid the risks of general anesthesia. The patient walks out of the surgery room within an hour of the procedure once the pain has been removed. And is able to return to normal daily activities within days of the procedure.
We have helped thousands of people who suffered from this condition, watch a patient testimonial for Spinal Stenosis
We encourage you to contact us to request a no-obligation MRI review or discussion with one of our medical professionals. Find out why The Bonati Spine Procedures are considered to be among the world’s best solutions for spine problems.
The Bonati Spine Procedures may include an array of the following procedures:
FORAMINOTOMY/FORAMINECTOMY
A foraminotomy/foraminectomy is a decompression surgery performed in order to increase the space of the foramen and hollow out the passageway where the nerve roots exit the spinal canal. The procedure removes bone or tissue that obstructs the neuro-foramen and compresses the nerve roots leading to inflammation and radiating pain. The removal of part of the lamina is often necessary for the surgeon to gain access to the affected nerve roots in the neuroforamen. For this reason, it is often performed in conjunction with a laminectomy or laminotomy.
LAMINECTOMY/ LAMINOTOMY
A laminectomy/laminotomy is a procedure performed to treat spinal stenosis. It is designed to relieve pressure off the spinal cord or nerve roots by opening up the spinal canal. The procedure is carried out by trimming part of the lamina (roof) of the vertebrae in the compressed area. The removal of part of the lamina creates an opening for the pinched nerves, relieving pressure on the nerve roots and reducing inflammation. The partial removal of the lamina may also allow the surgeon to remove any bone spurs or damaged tissue causing pain and inflammation in the patient.
DISCECTOMY
A discectomy is done to remove a portion of the disc that is putting pressure on the spinal cord or nerves.
FACETECTOMY
Facets are joints in your spine that help stabilize your spine. However, misaligned facet joints can put pressure on a nerve. In many cases, growth called bone spurs can develop.
FACET THERMAL ABLATION
A Facet Thermal Ablation is a laser eradication of sensory nerves causing pain. During a Bonati Facet Thermal Ablation (Rhizolysis), surgeons vaporize irritated and painful nerves around the facets of the vertebrae.
