Herniated Disc
Many people suffer from neck pain, back pain, or weakess in the extremities due to a herniated disc. Disc herniation most often takes place in the lower area of the spine (lumbar spine). Lumbar disc herniation occurs more often than cervical (neck) disc herniation. It is one of the most common causes lower back pain and sciatica.
Overview
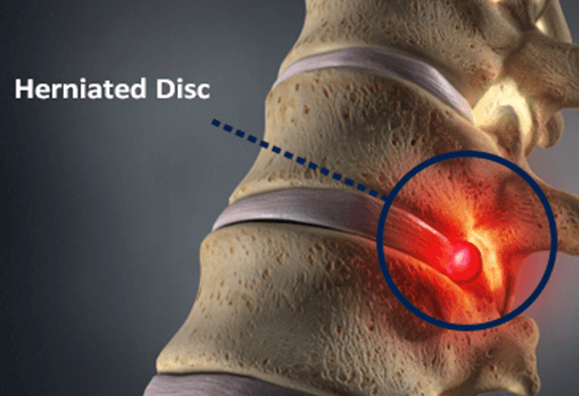
A herniated disc occurs when one of the discs located between the vertebrae in the spine gets damaged. These discs act as shock absorbers and keep the vertebrae from rubbing against each other. There are several terms used to describe disc pathology, including herniated disc, bulging disc, and pinched nerve.
Their symptoms are often similar. Medical professionals do not always agree on their definitions, frustrating patients trying to get a medical diagnosis. Adding to the confusion are an unusually wide range of terms also used to describe spinal disc problems, including slipped disc, ruptured disc, torn disc, collapsed disc, disc disease, disc protrusion, and black disc.
Anatomy
The spine consists of 33 vertebrae stacked on top of each other to form the spinal column. The spinal column supports the body and allows you to stand upright, bend, and twist without injury the spine. The spinal disc is a soft cushion that sits between each vertebra of the spine. The discs consist of an outer ring, the annulus, which has crisscrossing fibrous bands that attach to bodies of each vertebra. Inside each disc is a gel-filled center, called the nucleus pulposus.
The discs function like coiled springs. The crisscrossing configuration of the fibers of the annulus pull the vertebrae together and are cushioned by the elastic resistance of the nucleus. The nucleus allows the vertebrae to roll over the incompressible gel.
What is a Herniated Disc?
The discs become less elastic with age and more vulnerable to injury. As the discs become less elastic, they can rupture due to stress on the body.
When a disc ruptures, a portion of the spinal disc pushes outside its normal boundary. When a disc bulges out, it pinches the spinal nerves that are located very close to the disc. Therefore, the spinal nerves and spinal cord can become compressed causing pain, numbness, weakness and other herniated disc symptoms.
There is normally enough extra space around the spinal cord and spinal nerves. However these structures become compressed if too much of the herniated disc is bulging. When you have a symptomatic herniated disc, it is the not the disc itself that is painful, but the pain caused by the disc pinching the nerve that causes you to feel pain. A herniated disc is also often referred to as a slipped disc.
Lumbar Herniated Disc
Lumbar herniated discs are a common problem. They most often affect people aged 35-50. While a lumbar herniated disc is painful, the symptoms do not usually last long. Approximately 90% of patients diagnosed with a lumbar herniated disc have no symptoms after 6 weeks.
It is not unusual to have a lumbar disc herniation and have no symptoms. The symptoms may be triggered by moving or lifting something heavy and/or twisting the lower back.
Rarely, a lumbar herniated disc can cause cauda equina syndrome, which is caused by compression of the cauda equina (a bundle of nerve roots at the bottom of spinal cord). Cauda equine is a serious condition that should be treated immediately. If cauda equina syndrome is not treated quickly, it may result in neurological and physical problems such as paralysis, impaired bowel or bladder control, and difficulty walking.
If non-surgical treatments such as exercise, physical therapy, and medications do not relieve your pain, lumbar spine surgery may be necessary.
Symptoms of Lumbar Herniated Discs
Herniated discs occur most often in the lumbar spine. They commonly inflame or press against a nearby nerve and cause pain to radiate along the length of the nerve. This is the most common cause of sciatica, pain that radiates down the leg along the sciatic nerve. Symptoms of lumbar herniated discs include:
- Leg pain: although the herniated disc is in the back, the leg pain is usually worse than the back pain. Pain that radiates down the back of the leg is called lumbar radiculopathy or sciatica.
- Nerve pain: sharp, shearing, electric, piecing or radicular pain is the most common symptom described for a herniated disc.
- Variable location of symptoms: depending on the degree of the herniation and where the disc herniates, patients may experience symptoms in the low back, buttock, back or front of the thigh, the calf, foot and/or toes. The symptoms generally affect only one side of the body.
- Neurological symptoms: tingling, numbness, pins-and-needles, and weakness in the leg, foot, and/or toes.
- Foot drop: patients may experience difficulty lifting the foot when standing or walking on the ball of the foot.
Cervical Herniated Disc
Although a cervical herniated disc can be caused by a neck injury, the symptoms usually start suddenly. A cervical herniated disc can cause pain, numbness and/or tingling as the disc material presses on a cervical nerve. The cervical vertebrae are smaller than other spinal discs, therefore there is not as much room for the nerves. This means a small cervical herniated disc can cause severe pain. This pain may get worse with coughing, straining or laughing.
Whiplash due to an auto accident is a common cause of a herniated disc in the neck. Bad posture is another common factor to the problems in the cervical spine, including a herniated disc. By the excessive use of smartphones these days, cervical problems have been rising. Smartphone users spend hours with their heads dropped down. This puts excessive stress and strain on the neck, which can cause many problems in the cervical spine.
If non-surgical treatments such as exercise, physical therapy, and medications do not relieve your pain, cervical spine surgery may be necessary.
Symptoms of Cervical Herniated Discs
When a herniated disc occurs in the cervical region, these symptoms are possible:
- Shoulder pain: deep pain near or over the shoulder blades on the affected side.
- Neck pain: pain in the neck, especially in the back and sides, is a common symptom of a herniated disc in the cervical spine. Spasm of the neck muscles may happen.
- Arm pain: a herniated disc in the cervical spine may cause radiating pain that shoots down the arms, causing pain, muscle weakness and tingling in the arms.
- Variable location of symptoms: the symptoms of a cervical herniated disc depend on where the disc is herniated, and depending on the location, patients may experience pain in their shoulder, arms, hands, fingers and even chest. The symptoms often affect only one side of the body.
- Neurological symptoms: tingling, numbness, pins-and-needles, and weakness in the arm, hand, and/or fingers.
Thoracic Herniated Disc
The most common symptom of a thoracic herniated disc is pain that is either isolated to the upper back or radiating down a single nerve root. The pain is usually worse when coughing or sneezing.
adicular pain is sometimes perceived to be in the belly or chest, which can confuse the medical diagnosis and lead to an assessment for heart, lungs, kidneys, and gastrointestinal disorders as well as non-spine musculoskeletal causes. There are also disorders of the spine itself that have similar symptoms, including spine fracture, tumor, infection, and certain metabolic disorders.
A thoracic herniated disc can also be present with myelopathy (spinal cord dysfunction) if it has herniated in the spinal cord area. These symptoms include difficulty walking and balancing, numbness below the area of compression, weakness in the legs, and bladder or bowel dysfunction.
The symptoms of a thoracic herniated disc correlate with the location and size of the herniation. The herniated disc may protrude centrally, laterally, or centro-laterally (back and to the side).
If non-surgical treatments such as exercise, physical therapy, and medications do not relieve your pain, thoracic spine surgery may be necessary.
Causes of Herniated Discs
Most herniated disc causes are from the gradual age-related wear and tear on the spine, called disc degeneration. Spinal discs lose some of their water content due to age. That makes them more likely to tear or rupture.
Most patients can’t pin down exactly what caused their herniated disc. Some causes include using your back muscle instead of your leg muscles when lifting heavy objects, twisting or turning while lifting, and rarely, a traumatic event such as a blow to the back or a fall.
Diagnosing Herniated Discs
Diagnosis for a herniated disc begins with a physical examination and medical history taken by a doctor. The doctor will ask about the type of pain, other medical conditions, such as osteoporosis, osteoarthritis, spinal arthritis, your work and home life, and your medical history.
The physician will also perform range of motion tests, check your vital signs, monitor the patient’s gait, and examine your spine. Imaging tests are required if there is signs of a more serious problem.
Risk Factors
While the pain associated with a herniated disc may seem sudden, it is generally the result of a gradual process. Spinal discs have high water content that helps them stay flexible. They begin to dry out as part of the normal aging process and lose their ability to effectively cushion the vertebrae. The discs’ strong outer layer becomes brittle and can crack and tear from even minor movements. Risk factors for herniated discs include:
- Age: most herniated discs occur between 35-50 years of age.
- Gender: men are more than twice as likely to herniate a disc.
- Physical work: jobs that entail lifting heavy loads as well as repetitive pulling, pushing, and twisting.
- Obesity: carrying excess weight increases stress on the spine and a herniated disc is 12 times more likely.<
- Smoking: nicotine speeds up degeneration because it limits blood flow to the discs and hampers healing.
- Family medical history: heredity is a factor in disc degeneration, and therefore in disc herniation caused by degeneration.
Examination and Tests
During the first visit to a doctor for a possible disc herniation, the patient undergoes a physical examination. The doctor asks about the intensity and duration of the pain, previous injuries or illnesses, back surgeries or procedures, work environment, and leisure activities. Other conditions that might be a cause of their symptoms are also considered. In addition, the doctor may order imaging tests such as:
- MRI (magnetic resonance imaging) to determine where the herniation has occurred.
- CT scan (computed tomography) is sometimes used in place of an MRI if there is a reason that an MRI is not advised.
- X-rays are used to rule out issues such as broken bones, bone abnormalities, tumor, infection, or alignment problems of the spine.
- CT myelogram is similar to a CT scan but it uses dye in the spinal fluid with x-rays to view the dye. This can give the doctor a detailed view of the location and size of the herniation.
- Electromyography is used to identify the exact nerve that is affected.
Treatment for Herniated Discs
Herniated disc treatment depends on the severity of the condition and symptoms.
Non-Surgical Treatment
Non-surgical treatment includes one or more of the following: strengthening exercises or stretching, pain medication, and physical therapy. A physical therapist will give you exercises to strengthen your muscles and positions that can minimize the pain. Medications used to treat herniated discs may include:
- Over-the-counter (OTC) pain medications for mild to moderate pain.
- Anticonvulsants to treat radiating nerve pain.
- Muscle relaxants for muscle spasms.
- Antidepressants to reduce pain and restore normal sleep patterns.
- Cortisone injections to reduce inflammation directly in the area of nerve root pain and around the spinal nerves.
- Narcotics or opioids are prescribed for a short period of time to relieve pain that doesn’t improve with OTC drugs. It must be noted that, there is no solid evidence that opioids, or narcotics, work better than non-narcotic pain medications in relieving chronic pain from a spine condition. There are a number of serious risks with opioids that need to be considered. Opioids can be habit-forming if the patient isn’t careful. Opioids can also have limited effectiveness if the patient develops a tolerance to the medication over time.
Surgical Treatment
If non-surgical treatments such as exercise, physical therapy, and medications do not relieve your pain, surgery may be necessary. The Bonati Spine Institute has been a leader in advanced spine surgery for decades, with more than 75,000 successful procedures performed.
The Bonati Spine Procedures achieve a very high patient satisfaction rate in the treatment of herniated discs. The doctors at The Bonati Spine Institute may perform an array of procedures for treating herniated discs including:
Discectomy for a Herniated Disc
A discectomy is done to remove a portion of the bulged or herniated disc, thus relieving pressure on the spinal nerves or spinal cord. The Bonati Discectomy is done using local anesthesia and Conscious IV Sedation, allowing the patient to be comfortable and responsive during the procedure.
Foraminotomy for a Herniated Disc
A foraminotomy is a decompression surgery done in order to increase the space of the foramen and hollow out the canal where the nerve roots exit the spinal canal. The procedure involves the removal of bone or tissue that obstructs the neuro-foramen and pinches the nerve roots leading to inflammation and radiating pain. The removal of part of the lamina is often necessary for the surgeon to gain access to the affected nerve roots in the neuro-foramen.
Laminectomy/ Laminotomy for a Herniated Disc
A laminectomy/laminotomy is a procedure done to treat a herniated disc. The surgery is designed to relieve pressure on the spinal cord or spinal nerve roots through the widening of the spinal canal. The procedure is carried out by removing or trimming part of the lamina (roof) of the vertebrae in the compressed area. The removal of part of the lamina creates an opening for the compressed nerves, relieving pressure on the nerve roots and reducing inflammation. The partial removal of the lamina may also allow the surgeon to remove any bone spurs or damaged tissue causing pain and inflammation in the patient.. Laminectomy/ laminotomy are often done in order to give the surgeon the proper space to perform the foraminotomy.
Prevention & Self-Care
The chances of a disc herniation increases with age, however there are some actions you can take to prevent it.
- Quit smoking
- Eat well and maintain a healthy weight
- Maintain good posture
- Lift and bend properly
- Reduce alcohol use
- Exercise
The Bonati Spine Institute’s procedures can return you to your normal activities earlier than other surgical alternatives. We advocate patients suffering from herniated discs to contact us to request a no-obligation MRI review or discussion with one of our spine surgeons to see if you are a candidate for the Bonati Spine Procedures. Find out why The Bonati Procedures are considered to be among the world’s best solutions when it comes to spine surgery.
