Prolapsed Disc
A prolapsed disc is also called a slipped disc. But no matter what you call it, it often causes severe lower back pain.
Spine surgery for prolapsed disc
Overview
Bouts of back pain are very common, in fact, 31 million people experience low back pain at any given time. While this back pain is sometimes caused by a minor problem in a muscle, ligament, or other structure in the back, it can also be caused by a prolapsed disc. Twice as many men than women develop a prolapsed or slipped disc and the condition generally arises between the ages of 30 and 50.
When a prolapsed or slipped disc puts pressure on a nerve root, it can cause pain and other symptoms in the extremities innervated by the compressed nerve root. Sometimes, the symptoms resolve in several weeks on their own, but often they linger for more than 6 weeks. If the symptoms persist and become either acute or chronic, surgery may be an option.
Anatomy
The spine consists of many small bones called vertebrae. The spine has 33 vertebrae: 7 cervical, 12 thoracic, 5 lumbar, 5 fused sacral vertebrae, and 4 often fused coccygeal vertebrae.
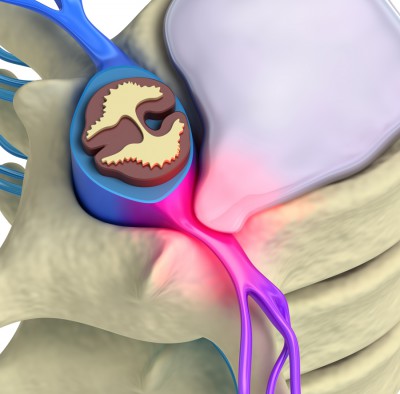
Between each of the 24 presacral vertebrae (cervical, thoracic, and lumbar) there is an intervertebral disc made up of strong rubber-like material (annulus fibrosus). Each intervertebral disc has a soft, jelly-like interior called the nucleus pulposus surrounded by a strong outer ring of fibrous tissue. The discs cushion the vertebrae and allow the spine to be flexible.
The spine houses the spinal cord, which is composed of the nerves that come from the brain and then branch out between the vertebrae to pass messages to and from the brain to various parts of the body, including the extremities.
Strong ligaments attached to the vertebrae provide extra strength and support to the spine, thus further protecting the spinal cord. In addition, various muscles are also attached to, and surround, the spine.
What Is a Prolapsed Disc?
Although a prolapsed disc is often referred to as a “slipped” disc, this is a misnomer. The disc doesn’t actually slip. What occurs is that the nucleus pulposus – the soft inner center of the disc – pushes or bulges out through a weakness in the fibrous outer part of the disc. This is also often called a herniated disc.
When the prolapsed disc presses on nearby structures of the spine, such as a nerve exiting the spinal cord, it can cause back pain and other symptoms. The sciatic nerve is the most commonly affected nerve. Usually, inflammation develops around the prolapsed disc, which can also cause back pain.
Where Does It Occur?
A disc prolapse can occur in any of the 24 presacral vertebrae in the spine. However, a disc prolapse is most likely to occur in the lumbar spine (lower back). In general, the larger the prolapse, the more severe and painful the symptoms.
Cervical Prolapsed Disc
Although disc prolapse is more common in the lower back, it can occur in the 7 vertebrae of the cervical spine. Levels C4 to C7 of the cervical spine are the most vulnerable to disc prolapse.
Lumbar Prolapsed Disc
Prolapsed lumbar discs are by far the most common. This condition is also sometimes called a ruptured, herniated, or slipped disc. It is most often caused by age-related deterioration in the spine. A prolapsed disc can happen at any age but becomes more likely after the age of 35.
Thoracic Prolapsed Disc
Since the thoracic spine is the least mobile portion of the spine, it is the least common area for a prolapsed disc to occur. The symptoms of a thoracic prolapsed disc vary depending on where the prolapsed disc occurs. The prolapsed disc can impinge on either a nerve, nerve root or on the spinal cord itself. It can herniate in a central, lateral, or centro-lateral direction.
Causes of a Prolapsed Disc
Many things can trigger the nucleus pulposus to prolapse out through a weakness in the outer fibrous ring of a disc. Awkward bending, poor mechanics when lifting heavy items, or even sneezing may be enough to cause a disc prolapse in people who have a weakness in a disc.
Risk factors for developing a prolapsed disc include:
- Trauma that causes the vertebra to fracture
- A job that requires lots of lifting
- A job that requires a lot of sitting
- Weight-bearing sports or exercise
- Obesity
- Smoking
- Weight-bearing sports or exercise
- Weakness in the spine due to normal aging
Symptoms of a Prolapsed Disc
The symptoms of a prolapsed disc are generally specific to the area of the spine in which the prolapse has occurred. Although the symptoms may not include neck or back pain in some patients, such pain is common. The main symptoms are listed below.
- Numbness, tingling, or pins and needles in the extremities
- Pain in the buttocks or behind the shoulder blades
- Pain radiating down one or both arms or legs
- Weakness involving one or both arms or legs
Symptoms in severe cases may include loss of bowel or bladder control, numbness in the genital area, and impotence.
Cauda Equina Syndrome
Although rare, cauda equina syndrome is a serious nerve root problem that can be caused by a prolapsed disc. The nerves at the very bottom of the spinal cord become compressed. In addition to low back pain, the condition causes:
- Bowel and bladder control problems and function (inability to pass urine).
- Numbness in the saddle area around the back passage (anus).
- Weakness in one or both legs.
This syndrome is considered an emergency and requires urgent treatment to avoid permanent damage to the nerves in the bowel and bladder. If you develop these symptoms, see a doctor immediately.
Diagnosis
Your physician will begin with an assessment of your physical condition and review of your medical history. In some cases, no tests are needed and the symptoms will disappear in a few weeks. However, imaging tests such as x-rays, CT-scans, or MRIs might be required if your symptoms persist or are severe. These imaging studies can show the level of the spine where the disc is prolapsed and will be needed if your doctor recommends surgery.
Exams & Tests
Depending on your symptoms, your doctor may require one or more of the following tests during the physical exam:
- Nerve function in certain parts of the leg or arm
- Muscle strength
- Pain with motion or palpitation
After the physical exam, a diagnostic imaging test or tests may be ordered to rule out some conditions, confirm the diagnosis, or gather more information. These tests include:
- X-ray to rule out other conditions as the source of the symptoms
- CT scan to better visualize the affected disc and surrounding area
- MRI scan for an accurate assessment of the spinal nerves and anatomy
- Discogram to confirm which disc is causing the symptoms. This test is controversial and not all doctors use it.
Treatment for a Prolapsed Disc
Many people opt for non-surgical treatment for a prolapsed disc. Everyone is different and not all treatments work for all patients. If you are still suffering from acute or chronic pain that negatively impacts your daily life, surgery may be necessary.
Non-Surgical Treatment
Continue with your normal activities unless your pain is severe. In the past, resting until the pain subsided was recommended but we now know you are likely to recover faster if you stay active. Staying active also lowers your chances of developing chronic back pain. However, a general rule is to refrain from activities that cause severe pain.
Non-surgical treatment for a prolapsed disc may include:
- Moderate, low-impact exercise to strengthen the surrounding muscles
- Physical therapy, including massage, stretching, and thermotherapy
- Alternative treatments such as acupuncture
- Painkillers such as paracetamol or codeine
- Anti-inflammatory painkillers such as ibuprofen, naproxen, or diclofenac
- Muscle relaxants such as diazepam or carisoprodol
Surgical Treatment
If you have tried non-surgical treatment options and are still in pain, surgery may be necessary.
The Bonati Spine Institute offers an array of procedures to treat disc problems. These procedures may include:
- Foraminotomy/Foraminectomy
- Laminotomy/Laminectomy
- Discectomy
Prevention & Self-Care
Preventing a prolapsed disc requires avoiding behaviors that may lead to intervertebral disc degeneration. Some things can’t be avoided, such as degenerative disc disease due to normal aging. But there are ways to strengthen the neck and back as well as reduce deterioration of the spine.
- Maintain a healthy weight
- Exercise regularly
- Stretch correctly
- Improve posture while standing, sitting, and sleeping
- Avoid excess alcohol consumption
- Quit smoking
- Use proper lifting techniques
