A new study published in the September 2019 journal SPINE revealed preoperative chronic opioid therapy negatively impacts long-term outcomes following cervical fusion surgery.
Below are study details and result excerpts as reported by Medscape.
Objective: The aim of this study was to define the impact of preoperative chronic opioid therapy (COT) on outcomes following cervical spine fusions.
Summary of Background Data: Opioid therapy is a commonly practiced method to control acute postoperative pain. However, concerns exist relating to use of prescription opioids, including inherent risk of abuse, tolerance, and inferior outcomes following major surgery.
Methods: A commercial dataset was queried from 2007 to 2015 for patients undergoing primary cervical spine arthrodesis, or fusion. Primary outcome measures were 1-year and 2-year reoperation rates, emergency department (ED) visits, adverse events, and prolonged postoperative opioid use.
Secondary outcomes included short-term outcomes including 90-day complications (cardiac, renal, neurologic, infectious, etc.). COT was defined as a history of opioid prescription filling within 3 months before surgery and was the primary exposure variable of interest.
Results: Overall, 20,730 patients (51.3% of participants were female; 85.9% of participants were over 50 years old) underwent primary cervical spine arthrodesis. Specifically, most patients (86%) underwent anterior cervical discectomy and fusion, while 11.6% underwent posterior cervical fusion.
Of these, 10,539 (or 50.8%) met criteria for COT.
Postoperatively, 75.3% remained on opioids at 3 months and 29.8% remained on opioids at 1 year. Multivariable models identified an association between COT and an increased risk of 90-day ED visit and wound complications.
At 1 year, COT was strongly associated with reoperations, ED visits, and adverse events including wound complications, infections, constipation, neurological complications, acute renal failure, and venous thromboembolism.
At 2 years, COT remained a significant risk factor for additional long-term negative outcomes such as reoperations, including adjacent segment disc disease, ED visits, and other adverse events. Preoperative COT was associated with prolonged postoperative narcotic use at 3 months, 1 year, and at 2 years after cervical arthrodesis.
Discussion: With the increase in awareness of the opioid epidemic, a number of new policies have been proposed and implemented at federal, state, and local levels. The impact of the epidemic varies largely throughout the country, and an evidence-based approach is necessary to guide changes in policy.
Within this study, the authors have categorized the negative short- and long-term impact that perioperative opioid use has on outcomes following cervical spine surgery. According to the findings, opioid medications have a broad range of effects on surgical outcomes, including readmissions, reoperations, ED visits, and many other adverse events. COT patients also have more complex postoperative pain needs, as evidenced by higher rates of spine injections at 1 and 2 years. They also found that in spite of surgical interventions, a large percentage of patients remain on prolonged opioid treatment. Several of these findings merit further discussion.
Conclusion: Preoperative chronic opioid therapy (COT) is a modifiable risk factor that is strongly associated with prolonged postoperative opioid use. In addition, COT was associated with inferior short-term and long-term outcomes after cervical spine fusion.
there is help without fusion and without opioids
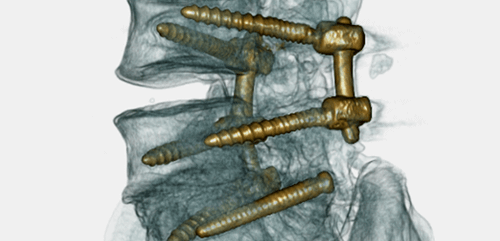
The Bonati Spine Institute does not believe in opioid therapy as a form or preoperative or postoperative treatment, nor do we perform fusion surgeries, or surgeries where hardware or devices of any kind are inserted into the spine. Our patented and outpatient procedures were created by Dr. Bonati as an alternative to these harsh surgeries. The tools and techniques, like conscious IV sedation, very small incisions, dialating tubes and FDA approved laser technology, allow patients to feel immediate results with a significantly reduced recovery time and often times, almost no need for postoperative pain medications. If you’re taking opioids as a long-term form of relief from spine-related pain, allow our surgeons to review your case and verify if our exclusive procedures might be able to help you. Simply call us at 855-267-0482 or complete our contact form and our patient advocates will contact you directly.
Read the full Medscape article here: https://www.medscape.com/viewarticle/917910
Read the full SPINE study here: https://www.ncbi.nlm.nih.gov/pubmed/30973507