Nearly all groups of patients with spinal stenosis — but not smokers — do better with surgery than with non-surgical treatment, reports a study in the October 1 issue of Spine. With the exception of smokers, patients who met strict inclusion criteria improved more with surgery than with non-operative treatment according to a study by The Dartmouth Institute for Health Policy and Clinical Practice.
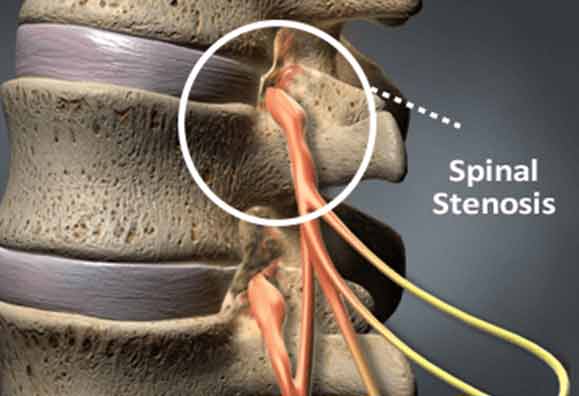
The research concentrated on patients with lumbar spinal stenosis, that being the most prevalent of spine disorders. Spinal stenosis is the narrowing of the spinal canal. It can occur in the lower (lumbar) or upper (cervical or neck area) spine. Narrowing of the spinal canal can put pressure on the spinal cord and nerve roots. This pressure, or pinching, can cause pain, weakness or numbness in the legs, feet or buttocks. It is estimated that 400,000 Americans suffer from leg pain and/or low back pain from lumbar spinal stenosis. The average age for surgery is 40-45 years, men are twice as likely to need lumbar stenosis surgery as women, and more than 95% of disk operations are performed on the fourth and fifth lumbar vertebrae.
The symptoms of lumbar stenosis generally develop slowly over time and symptoms may come and go. Lumbar stenosis symptoms may include:
-
Leg pain
-
Leg pain with walking
-
Tingling, weakness or numbness that radiates from the lower back into the buttocks and legs.
As lumbar spinal stenosis symptoms worsen, they may become quite debilitating. In the study, 419 patients with spinal stenosis underwent surgery while 235 received non-surgical treatment care. The results consistently showed greater improvement after surgery. The research was designed to increase the scientific evidence for decisions about treatment for spinal disorders.
The finding that most patients with spinal stenosis do better with surgery — including those with initially lower disability — contrasts with the “conventional wisdom” that surgery is most appropriate for patients with the worst initial symptoms. The results apply to patients experiencing persistent symptoms with imaging studies to confirm narrowing of the spinal canal.
The most striking finding is the importance of smoking — with smokers getting about the same improvement with or without surgery. The report’s conclusions advise that smoking cessation should be considered prior to surgery for spinal stenosis.
The findings also highlight the importance of considering individual characteristics when making treatment decisions — with patients participating in the decision as much as possible. These data can be used to help patients and surgeons individualize shared decision making discussions about likely outcomes following surgical or non-operative treatment for spinal stenosis.
Surgery for lumbar spinal stenosis should be considered if a patient’s ability to participate in everyday activities is unacceptably reduced and a concerted effort to relieve symptoms through non operative means has been unproductive. The bottom line is that the time to see a surgeon about surgery for spinal stenosis, or for any progressive spinal disorder, is when you are unhappy with a restricted activity level, and you’ve tried reasonable non-operative treatments (like anti-inflammatory medication, physiotherapy, and epidural steroid injection).
Patients facing surgery for spinal stenosis are no longer limited to the use of highly invasive open back surgery techniques, with such as options as the Bonati Spine Procedures producing far fewer complications, and requiring less time for recovery than traditional surgery which may require months of bed rest. Patients who choose advanced options such as the Bonati Spine Procedures experience shorter recovery times, no hospital stay, less anesthesia, and minimal or no scarring.
Patients choosing this option are often able to experience recovery the same day or a few days post -surgery and may be able to resume normal activities within weeks of surgery rather than having to wait months. This can help reduce the associated costs of spine surgery such as time away from work, paying for childcare, animal care, and self-care, as well as medical bills including pain medications.
If a spinal disorder has been diagnosed on an MRI scan or CT-myelogram, then a surgeon may discuss surgical options with you. For those who choose surgery for lumbar spinal stenosis, the good news is that lumbar laminectomy, the most common surgery for spinal stenosis, has a high success rate. Also in most cases lumbar decompression surgery allows people to return to a more active and pain free lifestyle. Some key considerations to help with the decision for surgery for a spinal problem, such as lumbar spinal stenosis, include that:
-
Spinal stenosis is generally not progressive. The pain tends to come and go, but it usually does not progress with time. The natural history with spinal stenosis, in the majority of patients, is that of episodic periods of pain and dysfunction.
-
A patient will usually do as well having lumbar stenosis surgery sooner as he or she would if the surgery were done later.
-
In the event of progressive weakness in the legs, then spinal stenosis surgery should be considered on an urgent basis rather than delayed in order to reduce the chance of long term nerve damage.
-
De-compressive surgery such as a lumbar laminectomy for spinal stenosis generally has a good success rate for relief of leg pain and leg symptoms (such as ability to walk) and activity-related lower back pain.
-
Potential risks of the surgery for lumbar stenosis are greatly affected by the general health of the patient, such as diabetes, obesity, or cigarette smoking. Similarly, if the proposed surgery is more involved (e.g. if it includes a spinal fusion with or without instrumentation), the risks of the surgery increase.