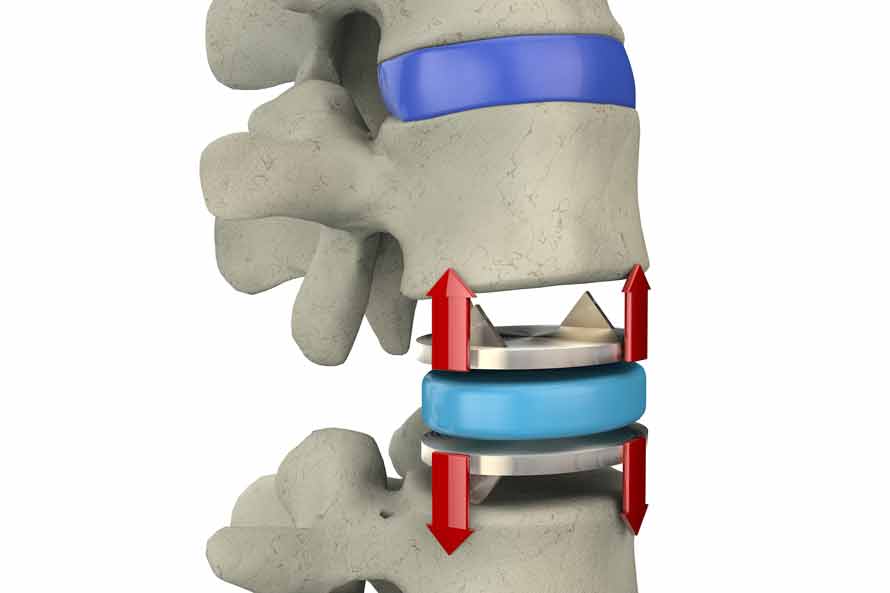
Lately there has been a considerable amount of debate about artificial spinal discs. Having an artificial spinal disc implanted is a major surgical procedure, and surgical treatment with an artificial disc is not without risk. A variety of complications may occur, either alone or in combination. Potential complications associated with spine surgery and artificial discs may include an allergic reaction to the implant material, implanted discs bending, breaking, loosening, or moving, and nerve or spinal cord impairment. Disc breakage or dislocation would require further surgery.
Additional complications from implanting artificial discs could include tearing of the protective membrane, the dura, that covers the spinal cord causing cerebrospinal fluid to leak, blood clots and blood flow restrictions, possibly resulting in stroke and the Inability to resume activities of normal daily living. There is also the risk that this surgical procedure will not be effective, and may not relieve or may cause worsening of preoperative symptoms.
Preferred patients for artificial disc implant are very limited to people with only one faulty disc and who do not have bones weakened from aging or degenerative changes. However, even with these restrictions in place, researchers writing in the European Spine Journal, looked at nearly 15 years of data from several studies and found a complication rate for implanted artificial discs of over 50%.
The man-made disc might wear out in a few years and need replacement. The load placed on the metal disc from the lumbar spine, (especially from overweight people) can accelerate wear and damage to the disc. Revision surgery to replace the damaged artificial disc in the lumbar area usually involves removing the artificial disc and then fusing the vertebrae above and below. Fusion spine surgery is viewed by most surgeons as complex and carries a success rate of approximately 50%.
Another issue to replacing a damaged disc with an artificial disc is whether the damaged disc is in the cervical (neck) region or the lumbar (lower back) region. Lumbar artificial discs are placed through an incision in the abdomen requiring the organs to be moved to one side. Even though artificial spine discs are also placed through the front of the neck, that area is seen as more accessible in surgery than the front of the lumbar spine.
Because of the weight of the body and the rotational stress that the trunk places on discs in the lumbar area, more stress is placed on artificial discs in the lumbar area vs. the cervical area, which only supports the weight of the head. Many spine surgeons, consequently, limit artificial disc implementation for the cervical spine only, even though disc degeneration and abnormalities in the lumbar spine are far more common. So even if a revision surgery were required, it would be easier to do on the neck than lumbar area. Yet, because scar tissue sets in after the initial surgery, it’s more difficult the second time to move the major veins and arteries that block access to the spine
Since lumbar artificial total disc replacement is unproven for the treatment of single or multiple level degenerative disc disease in skeletally mature patients, many insurance companies still consider the artificial spine disc an experimental or unproven procedure and therefore may not provide full coverage or any coverage at all. At the same time, the Centers for Medicare and Medicaid Services (CMS) has found that lumbar artificial disc replacement “is not reasonable and necessary”. All of this underscores how important it is for the patient to be well informed and well aware of the options to artificial discs available.
The Bonati Spine Institute offers a gentle patented procedure for relief from the pain caused by herniated or bulging discs, pinched nerves, spinal stenosis, sciatica and many other degenerative spine conditions. For more information call 855-267-0482 or complete our online form and our patient advocates will follow up with you directly.